Published 25 August 2023
Putting an End to the Itch: Essential Hives Relief Tips Revealed
Understanding Hives
To effectively manage hives and find relief, it’s important to understand the condition and its triggers. Let’s explore what hives are and some common triggers that can lead to their occurrence.
What are Hives?
Hives, also known as urticaria, are a common allergic reaction that appears as raised, itchy welts on the skin. They can vary in size and shape and often appear in clusters. Hives are typically red or pink in color and can be accompanied by swelling.
Hives occur when certain substances, known as allergens, trigger a release of histamine and other chemicals in the body. This release causes the blood vessels to leak fluid, resulting in the characteristic swelling and itching. Hives can appear suddenly and disappear within hours or persist for several weeks, depending on the underlying cause.
Common Triggers for Hives
Hives can be triggered by a variety of factors, including allergens, environmental factors, and underlying health conditions. Some common triggers for hives include:
-
Allergens: Allergens such as pollen, pet dander, certain foods, insect bites, or medications can trigger hives in susceptible individuals. Allergy testing for hives can help identify specific allergens.
-
Physical Factors: Exposure to certain physical factors like heat, cold, pressure, or sunlight can cause hives. This condition, known as physical urticaria, can be triggered by activities like exercise or exposure to cold water.
-
Stress and Emotions: Emotional stress and anxiety can sometimes trigger hives or worsen existing outbreaks. Stress-induced hives can be managed by finding effective stress management techniques.
-
Infections: Viral and bacterial infections, such as the common cold or urinary tract infections, can sometimes lead to hives. Viral infections and hives are often interlinked.
-
Medications: Some medications, including antibiotics, nonsteroidal anti-inflammatory drugs (NSAIDs), and certain pain relievers, can trigger hives as an allergic reaction. If you suspect a medication is causing your hives, consult with a healthcare professional.
-
Underlying Health Conditions: Hives can sometimes be a symptom of underlying health conditions, such as autoimmune disorders or thyroid disease. Autoimmune disorders and hives have been linked together.
Understanding the triggers for hives can help individuals effectively manage and prevent outbreaks. By identifying and avoiding the specific triggers that cause hives, individuals can significantly reduce their symptoms and improve their quality of life. For tips on managing hives and finding relief, continue reading the following sections.
Coping with Hives
For individuals experiencing hives, managing the uncomfortable symptoms is essential. Two key aspects of coping with hives are managing itchiness and reducing swelling and inflammation.
Managing Itchiness
Itchiness is a common and bothersome symptom of hives. Scratching hives can further irritate the skin and potentially lead to infection. To manage itchiness effectively, consider the following strategies:
-
Avoid scratching: Although it may provide temporary relief, scratching can worsen the itchiness and potentially damage the skin. Instead, gently pat or tap the affected areas to alleviate the itching sensation.
-
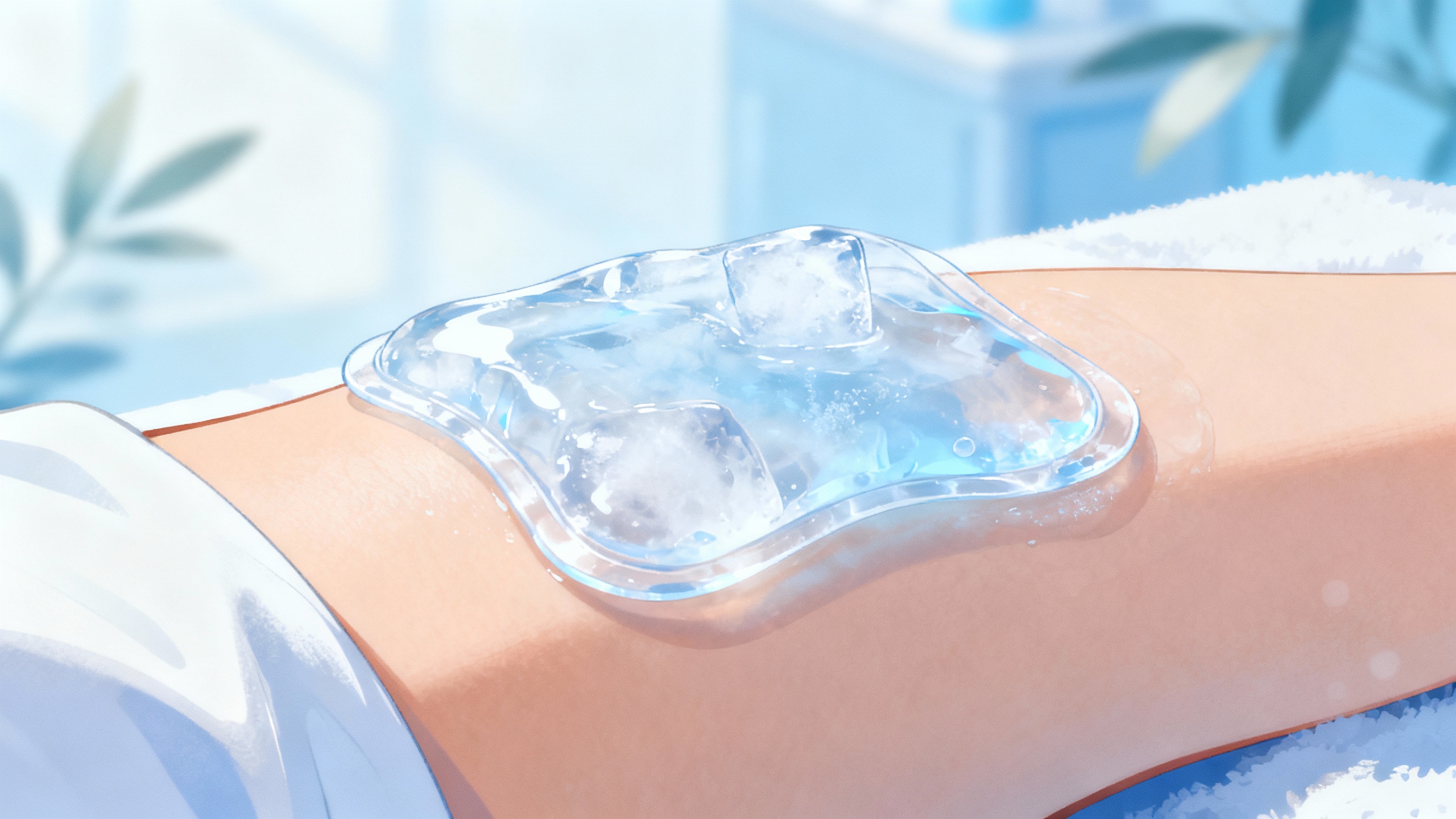
Apply cool compresses: Applying a cold compress to the hives can help soothe the itchiness and reduce inflammation. Wrap ice cubes in a clean cloth or use a cold gel pack, and gently press it against the affected areas for a few minutes at a time.
-
Take lukewarm baths: Taking lukewarm baths with colloidal oatmeal or baking soda can provide relief from itching. These ingredients help to soothe the skin and reduce irritation.
-
Use over-the-counter (OTC) antihistamines: OTC antihistamine medications can help alleviate itchiness caused by hives. These medications work by blocking the release of histamine, a chemical that triggers allergic reactions. It’s important to follow the recommended dosage and consult a healthcare professional if you have any underlying medical conditions or are taking other medications.
Reducing Swelling and Inflammation
Swelling and inflammation are common symptoms accompanying hives. To help reduce these symptoms, consider the following approaches:
-
Moisturize the skin: Keeping the skin well-moisturized can help prevent dryness and further irritation. Use fragrance-free, hypoallergenic moisturizers or emollients to hydrate the skin. Apply them generously after bathing or as needed throughout the day.
-
Try natural remedies: Some natural remedies, such as aloe vera gel or chamomile tea compresses, may help reduce swelling and inflammation associated with hives. However, it’s important to remember that natural remedies may not have scientific evidence supporting their effectiveness. If you choose to use natural remedies, conduct a patch test first to check for any adverse reactions and discontinue use if any irritation occurs.
By effectively managing itchiness and reducing swelling and inflammation, individuals with hives can find some relief. However, it’s important to note that these measures provide temporary relief and do not address the underlying cause of hives. If hives persist or worsen, it is recommended to consult a doctor to determine the appropriate course of action. For more information on seeking medical help for hives, refer to our article on when to consult a doctor and prescription medications for hives.
Essential Hives Relief Tips
When dealing with hives, finding relief from the itchiness and discomfort is a top priority. Here are some essential tips to help you manage hives and alleviate your symptoms.
Avoiding Triggers
Identifying and avoiding triggers is an important step in managing hives. Keep a journal to track your hives outbreaks and note any potential triggers such as certain foods, medications, stress, or exposure to allergens. By avoiding these triggers, you may be able to prevent or minimize the occurrence of hives. For more information on understanding hives triggers, refer to our article on understanding hives triggers.
Applying Cold Compresses
Cold compresses can provide immediate relief from itching and help reduce swelling associated with hives. Wrap a few ice cubes in a clean cloth or use a cold gel pack and apply it to the affected areas for 10 to 15 minutes. The cold temperature helps numb the area and soothe the itchiness. Be sure to place a thin cloth between the ice pack and your skin to avoid frostbite or irritation.
Using OTC Antihistamines
Over-the-counter (OTC) antihistamine medications can help relieve itching and reduce hives symptoms. Antihistamines work by blocking the histamine, a key chemical involved in triggering hives. It’s important to follow the recommended dosage instructions and consult with a healthcare professional if you have any concerns or if your symptoms persist.
| Common OTC Antihistamines |
|---|
| Diphenhydramine (Benadryl) |
| Loratadine (Claritin) |
| Cetirizine (Zyrtec) |
| Fexofenadine (Allegra) |
Moisturizing the Skin
Keeping your skin moisturized can help ease the discomfort associated with hives. Use fragrance-free and gentle moisturizers that are suitable for sensitive skin. Apply the moisturizer after bathing or whenever your skin feels dry. Moisturizing can help soothe the itchiness and prevent excessive dryness, which can aggravate hives.
Trying Natural Remedies
Some individuals find relief from hives symptoms by using natural remedies. While scientific evidence is limited, these remedies may be worth trying. Examples include oatmeal baths, aloe vera gel, chamomile tea compresses, and witch hazel. Keep in mind that what works for one person may not work for another, so it’s important to find what works best for you.
Remember, these tips provide general guidance for managing hives symptoms, but it’s essential to consult with a healthcare professional for a proper diagnosis and personalized treatment plan. If your hives persist, worsen, or are accompanied by severe symptoms, it’s important to seek medical help. For more information on when to consult a doctor, refer to our article on when to consult a doctor for hives.
By implementing these essential hives relief tips, you can take steps towards managing your symptoms and finding the comfort you need. Explore additional articles on coping with hives, managing hives symptoms, and hives treatment options for a comprehensive understanding of hives and how to alleviate their effects.
Seeking Medical Help
In most cases, hives can be managed with self-care measures and over-the-counter remedies. However, there are situations where it is necessary to consult a doctor for further evaluation and treatment. Understanding when to seek medical help is essential for effective hives management.
When to Consult a Doctor
It is advisable to consult a doctor if:
-
Hives last for more than six weeks: If your hives persist for more than six weeks, you may be experiencing a condition known as chronic hives or chronic spontaneous urticaria. A doctor can help determine the underlying cause and recommend appropriate treatment options. Check out our article on managing chronic hives for more information.
-
Severe itching and discomfort: If the itching and discomfort from hives are severe and affecting your daily life, seeking medical advice is important. A doctor may prescribe stronger medications or recommend additional treatments to provide relief.
-
Hives are accompanied by other symptoms: If you experience symptoms such as difficulty breathing, swelling of the lips or tongue, or dizziness along with hives, it could be a sign of a more serious allergic reaction. This condition, known as angioedema, requires immediate medical attention.
-
Hives are recurring or frequently reoccur: If you frequently experience hives outbreaks, it may be necessary to consult a doctor to identify triggers and develop a management plan. Allergy testing may be recommended to determine if an underlying allergy is causing the hives. Check out our article on allergy testing for hives for more information.
-
Hives are interfering with your daily life: If hives are significantly impacting your quality of life, causing emotional distress, or affecting your ability to carry out daily activities, seeking medical help can provide you with the necessary support and guidance to manage the condition effectively.
Prescription Medications for Hives
In cases where self-care measures and over-the-counter options are not providing sufficient relief, a doctor may prescribe prescription medications to help manage hives symptoms. These medications may include:
-
Antihistamines: Prescription-strength antihistamines can be more effective in relieving itching and reducing hives. They work by blocking the effects of histamine, a chemical released during an allergic reaction. Your doctor may recommend specific antihistamines based on your individual needs.
-
Corticosteroids: In severe cases of hives, corticosteroids may be prescribed for a short period to reduce inflammation and relieve symptoms. These medications should be used under the supervision of a healthcare professional due to their potential side effects.
-
Immunosuppressants: In certain situations, when hives are not responding to other treatments, immunosuppressant medications may be prescribed. These medications work by suppressing the immune system response that triggers hives.
It’s important to follow your doctor’s guidance and take prescribed medications as directed. They will assess your specific situation and recommend the most appropriate treatment options. Remember, seeking medical help is essential for proper diagnosis and management of hives.
