Published 25 August 2023
The Battle Within: Understanding Autoimmune Disorders and Hives
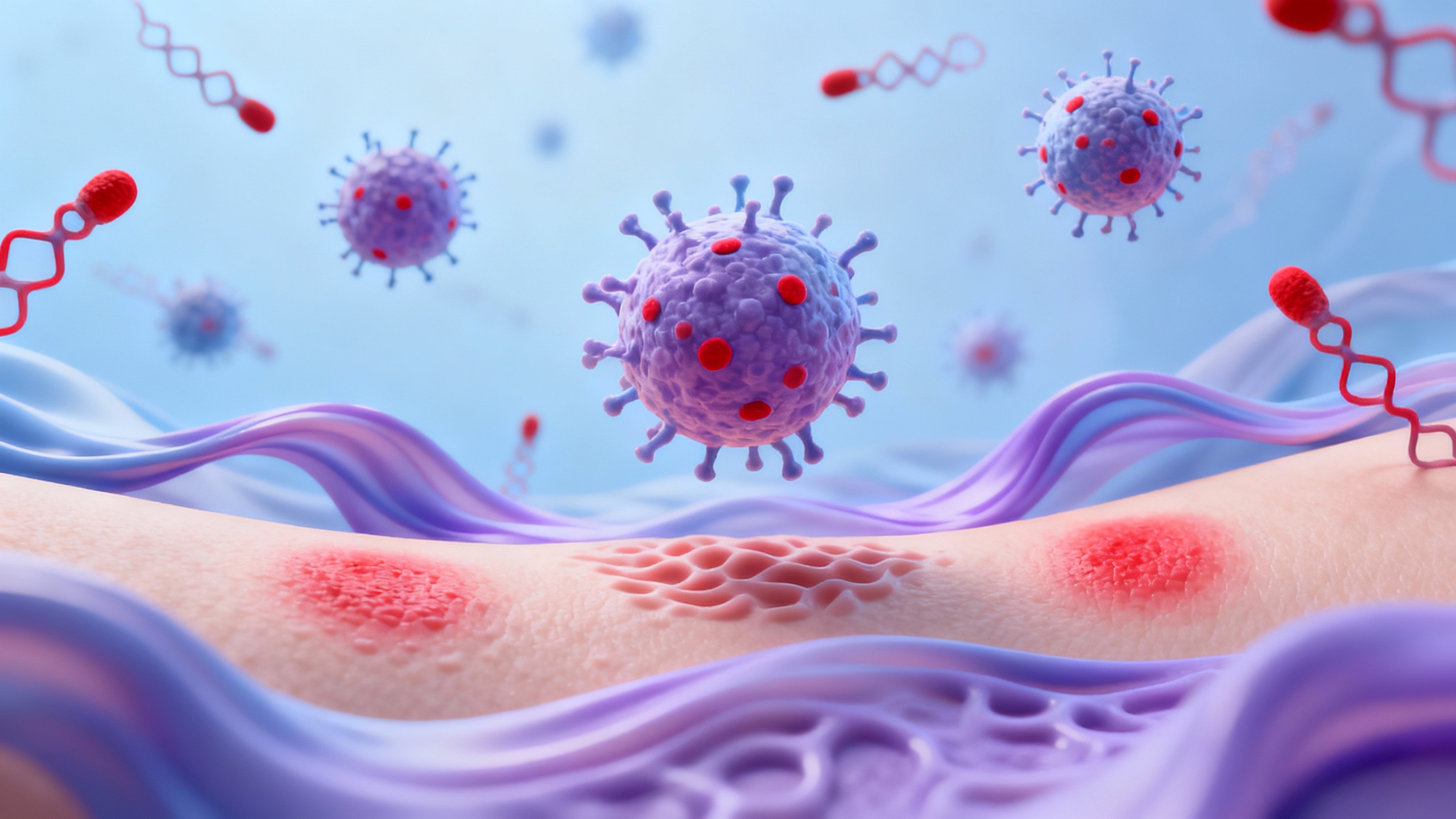
Unraveling the Connection: Autoimmune Disorders and Hives
Understanding the relationship between autoimmune disorders and hives can provide valuable insights into the underlying causes and management of these conditions.
Understanding Autoimmune Disorders
Autoimmune disorders are conditions where the immune system mistakenly attacks healthy cells and tissues in the body. Instead of targeting foreign invaders, the immune system becomes overactive and starts attacking its own cells. This abnormal immune response can lead to inflammation and damage in various organs and systems.
There are numerous autoimmune disorders, each affecting different parts of the body. Some common autoimmune disorders include rheumatoid arthritis, systemic lupus erythematosus, and psoriasis. It is important to note that autoimmune disorders vary in their symptoms, severity, and impact on overall health.
What are Hives?
Hives, also known as urticaria, are raised, itchy welts that appear on the skin. They can vary in size and shape and often develop suddenly. Hives occur when cells in the skin release histamine and other chemicals, causing blood vessels to leak fluid. This fluid accumulates in the skin, resulting in the characteristic red, swollen, and itchy patches.
Hives can be acute or chronic. Acute hives last for a short period of time, typically less than six weeks, and are often triggered by allergies or viral infections. Chronic hives, on the other hand, persist for longer than six weeks and may have underlying causes such as autoimmune disorders.
The exact relationship between autoimmune disorders and hives is complex and not fully understood. However, it is believed that autoimmune dysfunction can contribute to the development of chronic hives in some individuals. In these cases, the immune system may mistakenly identify certain substances in the body as threats, triggering the release of histamine and the onset of hives.
By unraveling the connection between autoimmune disorders and hives, individuals experiencing hives can gain a better understanding of their condition and work with healthcare professionals to develop an appropriate management plan. It is important to consult a healthcare provider for a proper diagnosis and to explore appropriate treatment options.
In the following sections, we will explore the specific autoimmune disorders that can cause hives and delve deeper into the mechanism behind hives in autoimmune disorders.
The Link between Autoimmune Disorders and Hives
While hives can occur for various reasons, one notable association is the link between autoimmune disorders and hives. Autoimmune disorders are conditions in which the body’s immune system mistakenly attacks its own healthy cells. This immune dysfunction can trigger a range of symptoms, including hives.
Autoimmune Disorders that Can Cause Hives
Several autoimmune disorders have been linked to the development of hives. Some of the common autoimmune conditions that can cause hives include:
-
Hashimoto’s thyroiditis: This autoimmune disorder affects the thyroid gland, leading to an underactive thyroid. Hives may occur as a result of the immune system’s reaction to the thyroid dysfunction.
-
Systemic lupus erythematosus: Lupus is a chronic autoimmune disease that can affect multiple organs and systems within the body. Hives are one of the possible dermatological manifestations of lupus.
-
Rheumatoid arthritis: This autoimmune condition primarily affects the joints, causing inflammation and pain. Hives can sometimes occur as an associated symptom.
-
Celiac disease: Celiac disease is an autoimmune disorder characterized by an intolerance to gluten. In some cases, hives may be triggered by the immune response to gluten ingestion.
-
Type 1 diabetes: Hives have been observed in individuals with type 1 diabetes, an autoimmune condition in which the immune system attacks the insulin-producing cells in the pancreas.
Mechanism of Hives in Autoimmune Disorders
The exact mechanism by which autoimmune disorders lead to the development of hives is not fully understood. However, researchers believe that the immune system’s dysregulation and overactivity in autoimmune conditions can trigger the release of histamine and other inflammatory substances. This release of histamine causes the blood vessels in the skin to leak fluid, resulting in the characteristic red, itchy welts of hives.
It’s important to note that hives can also occur independently of autoimmune disorders, and not everyone with an autoimmune condition will experience hives. If you suspect that your hives may be related to an underlying autoimmune disorder, it’s essential to consult with a healthcare professional for accurate diagnosis and appropriate management.
In the next section, we will explore strategies for managing hives in the context of autoimmune disorders, including identifying triggers, medications, and lifestyle changes. For more information on hives and related topics, refer to our articles on managing hives symptoms and reducing hives swelling.
Managing Hives in Autoimmune Disorders
When it comes to managing hives in the context of autoimmune disorders, there are several approaches that can be taken to alleviate symptoms and minimize flare-ups. These include identifying triggers and allergens, medications and treatments for hives, and lifestyle changes that can help reduce the frequency and severity of hives outbreaks.
Identifying Triggers and Allergens
One of the first steps in managing hives is to identify and avoid triggers and allergens that may be contributing to the development of hives. Common triggers include certain foods, medications, insect bites, pollen, and environmental factors. It is important to keep a record of any potential triggers and allergens that may be associated with hives outbreaks. Allergy testing can also be helpful in identifying specific allergens that may be causing hives. For more information on allergy testing, check out our article on allergy testing for hives.
Medications and Treatments for Hives
There are several medications and treatments available that can help relieve the symptoms of hives. Antihistamines are commonly used to reduce itching and inflammation associated with hives. They work by blocking the effects of histamine, a chemical that is released during an allergic reaction. In more severe cases of hives, corticosteroids may be prescribed to reduce inflammation and provide relief. Other treatment options include creams or ointments containing ingredients like calamine or menthol, which can soothe the skin and alleviate itching. For a comprehensive understanding of hives treatment options, refer to our article on hives treatment options.
Lifestyle Changes to Minimize Hives
Making certain lifestyle changes can also help minimize hives outbreaks. It is important to maintain good overall health by eating a balanced diet, exercising regularly, and getting enough sleep. Stress management techniques, such as relaxation exercises or therapy, can also be beneficial, as stress can be a trigger for hives in some individuals. Additionally, taking steps to protect the skin from irritants and allergens, such as using gentle skincare products and avoiding excessive heat or cold, can help prevent hives outbreaks. For more tips on reducing hives swelling and managing symptoms, refer to our article on reducing hives swelling.
By implementing these strategies, individuals with autoimmune disorders can better manage their hives symptoms and improve their overall quality of life. It is important to work closely with a healthcare professional to determine the most appropriate management plan based on individual needs and medical history. Remember, while these approaches can help alleviate symptoms, it is essential to address the underlying autoimmune disorder with the guidance of a healthcare professional.
Coping and Finding Relief
Living with hives can be challenging, but there are strategies you can use to cope with the itch and discomfort. Finding relief involves a combination of soothing the itch, managing stress, and seeking support from professionals. Here are some tips to help you navigate the battle against hives:
Soothing the Itch and Discomfort
- Cool compresses: Applying cool compresses to the affected areas can help soothe the itchiness and reduce inflammation. You can use a cold towel or ice pack wrapped in a cloth to avoid direct contact with the skin.
- Anti-itch creams: Over-the-counter anti-itch creams or ointments containing ingredients like hydrocortisone or calamine can provide temporary relief from itching and help reduce redness.
- Oatmeal baths: Taking a soothing oatmeal bath can help relieve itching and calm irritated skin. Simply add colloidal oatmeal to lukewarm bathwater and soak for about 15 minutes.
- Avoid hot water: Hot water can exacerbate itching and dry out the skin, so it’s best to shower with lukewarm water instead.
- Moisturize: Keeping your skin moisturized can help alleviate dryness and reduce itchiness. Opt for fragrance-free and hypoallergenic moisturizers to minimize the risk of irritation.
- Avoid scratching: Although it can be tempting to scratch, try to resist the urge as it can worsen the symptoms and potentially lead to skin damage and infections.
Stress Management and Relaxation Techniques
- Stress reduction: Stress can trigger or worsen hives in some individuals. Engaging in stress reduction techniques such as deep breathing exercises, meditation, yoga, or engaging in hobbies can help manage stress levels and potentially alleviate hives.
- Relaxation techniques: Practicing relaxation techniques like progressive muscle relaxation or guided imagery can help divert your focus from the itch and promote a sense of calm.
- Exercise: Regular exercise can help reduce stress levels and release endorphins, which are natural mood boosters. However, be mindful of exercise-induced hives and take appropriate precautions if exercise triggers your hives.
Seeking Support and Professional Help
- Support groups: Connecting with others who experience similar challenges can provide emotional support and valuable insights. Consider joining online support groups or seeking local support groups for individuals with hives or autoimmune disorders.
- Professional help: If your hives persist or significantly impact your quality of life, it’s important to seek professional help. A dermatologist or allergist can help diagnose the underlying cause of your hives and recommend appropriate treatment options. They may suggest prescription medications or other interventions tailored to your specific needs.
Remember, finding relief from hives is a process that may require some trial and error. It’s essential to work closely with healthcare professionals to identify triggers, manage symptoms, and develop a personalized plan for coping with hives. For more tips on managing hives, check out our article on hives relief tips.
