Published 25 August 2023
Banishing the Bumps: Coping with Allergic Reactions and Hives
Understanding Allergic Reactions and Hives
To effectively cope with allergic reactions and hives, it is essential to have a clear understanding of these conditions. This section will provide an overview of what allergic reactions and hives are, as well as the causes and triggers of hives.
What are Allergic Reactions?
Allergic reactions occur when the immune system overreacts to substances that are usually harmless. These substances, known as allergens, can include pollen, pet dander, certain foods, or medications. When a person with allergies comes into contact with an allergen, their immune system releases chemicals, such as histamine, which can cause various symptoms. These symptoms can range from mild, such as sneezing and itching, to severe, such as difficulty breathing or anaphylaxis.
What are Hives?
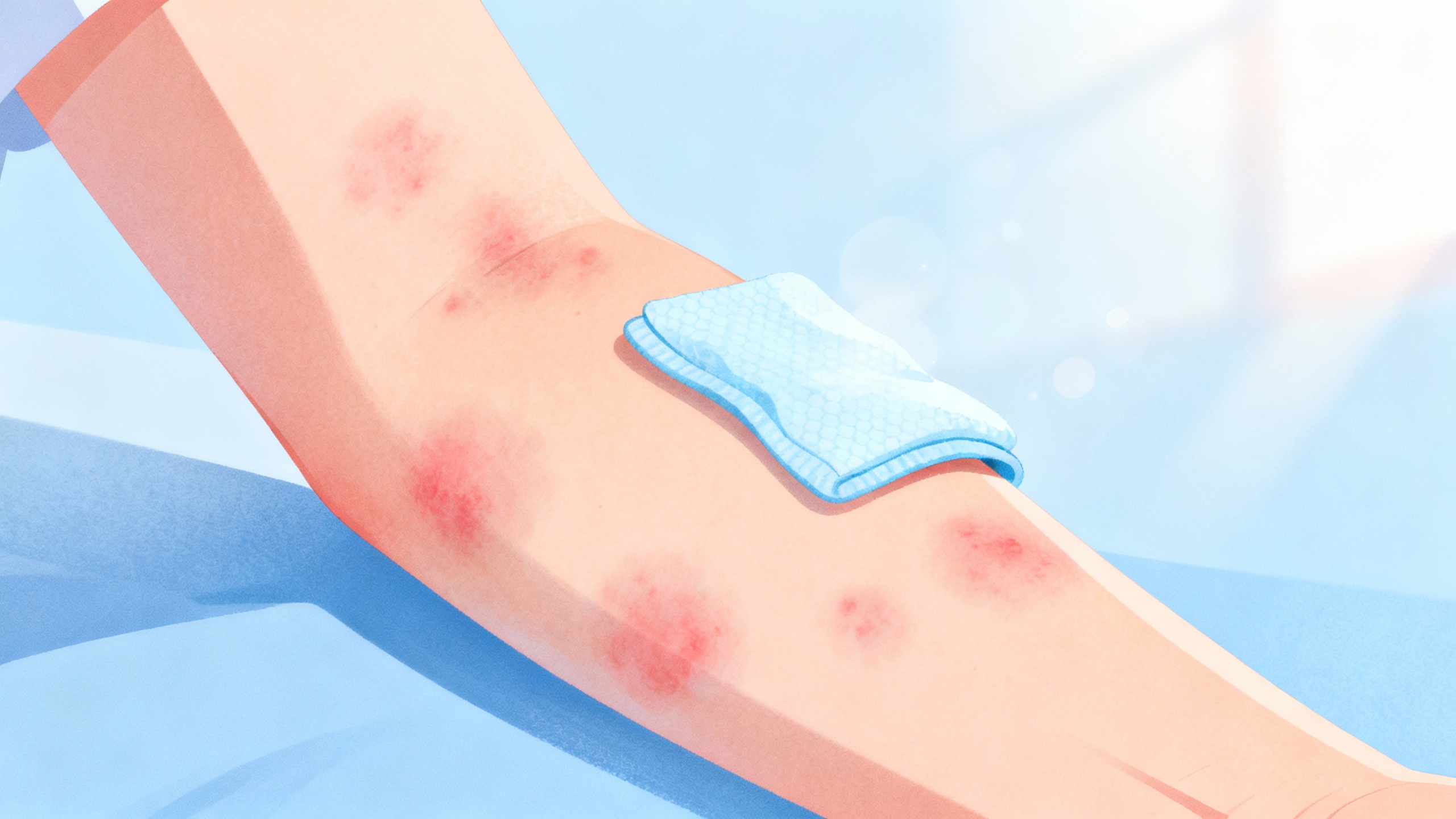
Hives, also known as urticaria, are a type of skin rash characterized by raised, itchy, and often red welts. They can appear anywhere on the body and vary in size and shape. Hives are typically caused by the release of histamine and other chemicals in response to an allergic reaction or other triggers. The welts can come and go, often moving around the body and lasting for a few hours to several days.
Causes and Triggers of Hives
Hives can be triggered by a range of factors, including:
- Allergens: Common allergens that can lead to hives include certain foods (e.g., nuts, shellfish, eggs), medications (e.g., antibiotics, NSAIDs), insect stings, and environmental factors (e.g., pollen, dust mites).
- Physical triggers: Some individuals may experience hives in response to physical stimuli, such as pressure on the skin (dermatographism), exposure to cold or heat, exercise, or sunlight.
- Infections: Certain viral or bacterial infections, such as the common cold or strep throat, can cause hives as an immune response.
- Underlying medical conditions: Hives can sometimes be associated with underlying medical conditions, such as autoimmune disorders, thyroid disease, or chronic infections.
- Stress and other triggers: Emotional stress, hormonal changes, certain food additives, or contact with irritants (e.g., chemicals, plants) can also trigger hives in susceptible individuals.
By understanding the causes and triggers of hives, individuals can take steps to identify and avoid potential allergens or stimuli that may lead to hives outbreaks. For more information on managing hives and seeking relief, continue reading our article on coping with hives.
Remember, while this information provides a general understanding of allergic reactions and hives, it is always important to consult with a healthcare professional for a proper diagnosis and personalized guidance.
Coping with Allergic Reactions and Hives
When dealing with allergic reactions and hives, it’s important to develop effective coping strategies to manage their symptoms and find relief. This section will explore two key aspects of coping with allergic reactions and hives: identifying and avoiding triggers and non-medical relief for hives.
Identifying and Avoiding Triggers
One of the first steps in managing hives is identifying the triggers that can cause or exacerbate your allergic reactions. Common triggers include certain foods, medications, insect bites, pollen, pet dander, and stress. By keeping a detailed record of your symptoms and daily activities, you can start to identify patterns and potential triggers. If you suspect a specific trigger, it may be helpful to consult with an allergist or dermatologist who can perform allergy testing to confirm your suspicions. For more information on allergy testing and its role in identifying hives triggers, refer to our article on allergy testing for hives.
Once you have identified your triggers, the next step is to avoid or minimize your exposure to them. This may involve making dietary changes, implementing preventive measures, or adjusting your lifestyle. For instance, if you have identified pollen as a trigger, you can monitor pollen forecasts and take precautions when outdoor pollen levels are high. Similarly, if stress triggers your hives, practicing stress management techniques such as meditation or yoga can be beneficial. By understanding and avoiding your triggers, you can significantly reduce the frequency and severity of your hives outbreaks.
Non-Medical Relief for Hives
In addition to avoiding triggers, there are several non-medical techniques that can provide relief for hives. These techniques are focused on soothing the skin, reducing inflammation, and minimizing discomfort. Here are some effective strategies:
Cooling the Skin
Applying cool compresses or taking cool showers can help relieve itching and reduce inflammation associated with hives. The cool temperature helps constrict blood vessels, providing temporary relief from itching and swelling. Remember to avoid hot water, as it can exacerbate symptoms and worsen hives.
Applying Calming Agents
There are various calming agents that can be applied topically to soothe the skin and alleviate itching. Some common options include calamine lotion, oatmeal baths, and aloe vera gel. These substances have anti-inflammatory properties and can provide temporary relief from hives symptoms. However, it’s essential to ensure that the products you choose are suitable for your skin type and do not contain any ingredients that may further irritate your skin.
Wearing Loose and Breathable Clothing
Choosing the right clothing can make a significant difference in managing hives. Opt for loose-fitting and breathable materials such as cotton or linen, which allow for better air circulation and reduce friction against the skin. Avoid tight-fitting clothing, as it can further irritate the skin and increase itching.
By embracing these non-medical relief techniques, you can find comfort and alleviate the symptoms associated with hives. However, it’s important to note that these strategies provide temporary relief and may not address the underlying cause of your hives. If you experience persistent or severe symptoms, it is advisable to seek medical attention and explore other treatment options. Our article on hives treatment options provides further information on medical interventions available for managing hives.
Understanding and implementing coping strategies for allergic reactions and hives can improve your quality of life and help you regain control over your symptoms. By identifying and avoiding triggers and utilizing non-medical relief techniques, you can effectively manage hives and find comfort amidst the bumps.
Seeking Medical Treatment
When it comes to managing allergic reactions and hives, sometimes it’s necessary to seek medical treatment for relief. Consulting a healthcare professional can help you navigate the best course of action based on the severity and frequency of your symptoms. In this section, we will explore when to consult a healthcare professional, over-the-counter options for relief, and prescription medications that may be prescribed for hives.
When to Consult a Healthcare Professional
If you are experiencing hives that are severe, persistent, or accompanied by other symptoms such as difficulty breathing or swelling of the lips and tongue, it is important to seek medical attention immediately. These symptoms may indicate a severe allergic reaction called anaphylaxis, which requires immediate medical intervention.
Additionally, if you are unsure about the cause of your hives, or if they are interfering with your daily life and causing significant discomfort, it is advisable to consult a healthcare professional. They can conduct a thorough evaluation, identify potential triggers, and recommend appropriate treatment options.
Over-the-Counter Options for Relief
For mild cases of hives, over-the-counter antihistamines can provide temporary relief from itching and help reduce the appearance of hives. Antihistamines work by blocking the release of histamine, a substance that contributes to allergic reactions and inflammation.
Here are some common over-the-counter antihistamines used for hives:
| Antihistamine | Brand Names |
|---|---|
| Diphenhydramine | Benadryl, Nytol |
| Cetirizine | Zyrtec |
| Loratadine | Claritin |
| Fexofenadine | Allegra |
It’s important to follow the recommended dosage instructions on the product packaging and consult with a healthcare professional if you have any underlying medical conditions or are taking other medications.
Prescription Medications for Hives
In cases where over-the-counter options are not providing adequate relief, a healthcare professional may prescribe prescription medications to manage hives. These medications are typically recommended for individuals with chronic or recurrent hives that persist for more than six weeks.
Some commonly prescribed medications for hives include:
| Medication | Type |
|---|---|
| Antihistamines | These prescription-strength antihistamines, such as hydroxyzine or levocetirizine, may provide more effective relief than over-the-counter options. |
| Corticosteroids | In severe cases, short courses of oral or injectable corticosteroids, such as prednisone, may be prescribed to reduce inflammation and alleviate symptoms. |
| Immunosuppressants | For individuals with chronic hives that do not respond to other treatments, immunosuppressant medications like cyclosporine may be considered to suppress the immune system’s response. |
It’s important to note that prescription medications should only be taken under the guidance and supervision of a healthcare professional, as they may have potential side effects and interactions with other medications.
By seeking medical treatment, individuals with hives can receive proper guidance, access effective medications, and alleviate symptoms more effectively. Remember, everyone’s experience with hives is unique, so it’s essential to consult a healthcare professional to determine the best course of treatment for your specific situation.
Managing Severe Allergic Reactions
In some cases, allergic reactions and hives can escalate to a severe level, requiring immediate attention and care. It’s crucial to be able to recognize the symptoms of anaphylaxis, understand how to administer epinephrine, and know when to seek emergency medical care.
Recognizing Anaphylaxis Symptoms
Anaphylaxis is a severe allergic reaction that can be life-threatening if not treated promptly. It typically involves a rapid onset of symptoms that affect multiple systems of the body. Some common symptoms of anaphylaxis include:
- Difficulty breathing, shortness of breath, or wheezing
- Swelling of the face, lips, tongue, or throat
- Hives or widespread skin redness and itching
- Tightness or pain in the chest
- Nausea, vomiting, or abdominal cramps
- Dizziness or lightheadedness
- Rapid or weak pulse
- Loss of consciousness
If you or someone around you experiences these symptoms after exposure to a known allergen or suspect an allergic reaction, it is essential to take immediate action.
Administering Epinephrine
Epinephrine, also known as adrenaline, is the primary treatment for anaphylaxis. It helps to reverse the symptoms and stabilize the body during a severe allergic reaction. If you or someone else is experiencing anaphylaxis, follow these steps:
- Call emergency services or ask someone nearby to do so. Time is of the essence during an anaphylactic reaction.
- Locate an epinephrine auto-injector, such as an EpiPen, if available. These devices are designed for easy and quick administration.
- Remove the safety cap from the auto-injector.
- Hold the auto-injector firmly against the thigh (through clothing if necessary) at a 90-degree angle.
- Press the device firmly against the thigh to activate the injection. Hold it in place for a few seconds to ensure the full dose is delivered.
- Seek immediate medical attention even after administering epinephrine. Anaphylaxis requires thorough medical evaluation and monitoring.
It’s important to note that epinephrine should only be administered if anaphylaxis is suspected or confirmed. If you are unsure whether the symptoms indicate anaphylaxis, it’s safer to err on the side of caution and seek medical attention.
Seeking Emergency Medical Care
After administering epinephrine, it is crucial to seek emergency medical care. Even if the symptoms subside or improve, a healthcare professional should evaluate the individual to assess the severity of the allergic reaction and provide further treatment if necessary.
Emergency medical care is vital as additional medications, such as antihistamines and corticosteroids, may be required to prevent a recurrence or progression of the reaction. Furthermore, healthcare professionals can monitor the individual for potential delayed reactions or complications.
Remember, anaphylaxis is a medical emergency, and prompt action is necessary to ensure the best possible outcome. Seeking immediate medical care is crucial in managing severe allergic reactions and preventing potentially life-threatening consequences.
For long-term management strategies to prevent allergic reactions and hives, consider exploring options such as allergy testing and immunotherapy, making lifestyle changes to manage allergies, and creating an emergency action plan. By taking a proactive approach, individuals can reduce the risk of severe allergic reactions and live a healthier, more comfortable life.
Long-Term Strategies for Prevention
While finding relief from allergic reactions and hives is essential, focusing on long-term strategies to prevent their occurrence can provide significant benefits. By addressing the underlying causes and triggers, individuals can reduce the frequency and severity of allergic reactions. This section explores three key strategies for long-term prevention: allergy testing and immunotherapy, lifestyle changes to manage allergies, and creating an emergency action plan.
Allergy Testing and Immunotherapy
To effectively manage allergic reactions and hives, it is crucial to identify the specific allergens that trigger them. Allergy testing, conducted by a healthcare professional, can help determine the substances that cause an allergic response in an individual. The tests may include skin prick tests, blood tests, or patch tests, depending on the suspected allergens.
Once the allergens are identified, immunotherapy may be recommended. This treatment involves gradually exposing the individual to increasing amounts of the allergen, helping the body develop a tolerance and reduce the severity of the allergic response over time. Immunotherapy can be administered through allergy shots or sublingual drops or tablets, depending on the specific allergens and the individual’s needs.
Lifestyle Changes to Manage Allergies
Making certain lifestyle changes can significantly contribute to managing allergic reactions and hives. Here are some tips to consider:
-
Avoiding Triggers: Take steps to minimize exposure to known allergens. This may involve avoiding specific foods, implementing dust mite covers on bedding, using hypoallergenic products, or keeping windows closed during high pollen seasons. For more information on understanding hives triggers, refer to our article on understanding hives triggers.
-
Maintaining a Healthy Diet: Consuming a balanced diet rich in nutrients may help support the immune system and reduce the likelihood of allergic reactions. However, if food allergies are a concern, it is crucial to identify and eliminate trigger foods. For more information, refer to our article on hives and food intolerance.
-
Reducing Stress: Stress can exacerbate allergic reactions and hives. Engaging in stress-reducing activities such as exercise, meditation, or hobbies can help manage stress levels. For more information, refer to our article on stress-induced hives.
Creating an Emergency Action Plan
Having an emergency action plan in place is vital for individuals prone to severe allergic reactions and hives. This plan outlines the necessary steps to be taken in case of an emergency and ensures that appropriate medical attention is sought promptly. The plan should include:
-
Emergency Contacts: List the names and contact information of healthcare professionals, emergency services, and family members who should be notified in case of an allergic emergency.
-
Medications and Dosages: Specify the medications that should be administered in case of an allergic reaction. Include the correct dosages and the method of administration, such as using an epinephrine auto-injector. For more information, refer to our article on administering epinephrine.
-
Triggers to Avoid: Identify specific triggers that should be avoided to prevent allergic reactions. This may include certain foods, medications, or environmental factors.
-
Emergency Action Instructions: Clearly outline the steps to be taken in case of an allergic reaction, including how to recognize the symptoms, when to administer medication, and when to seek emergency medical care. For more information, refer to our article on recognizing anaphylaxis symptoms.
By implementing these long-term strategies for prevention, individuals can take control of their allergic reactions and hives. Allergy testing, lifestyle changes, and emergency action plans can significantly reduce the impact and frequency of allergic episodes, providing individuals with a greater sense of comfort and well-being.
